REPORT SHINYANGA. TANZANIA 2018

We began our journey to Tanzania at the Barajas airport on 9th March 2018. We met a few hours before to pack the material and get to know the whole team. For some of us it´s the first experience as cooperators, others with some previous experience, but all with the same illusion that this type of missions entails. We invoice without problems 9 packages of 23Kg each one. A long trip awaits us, from Madrid to Addis Ababa (with a stop in Rome) and from there to Dar es-Salam, where we have to spend a night before leaving for our final destination, Shinyanga. At the airport we obtain the visa for entry into the country without problems, although after a long wait. We passed the customs with all the material without problems thanks to Dr Chacha, pediatrician in Shinyanga hospital, who comes to pick us up at the airport with all the necessary permits. We have more than 24h of travel, so we went to the hotel to leave all the luggage and go out to explore the city. The driver of the hotel takes us for a walk around the city, to a market of local crafts and finally to enjoy a pleasant dinner in a restaurant with terrace by the sea. The next day we know the fishing port and the market, where there is a frenetic activity with people cleaning and selling fish or cooking to eat there. There are also multiple stalls where they sell starfish, all kinds of shells of all shapes and colors imaginable. We also visit the national museum, a good place to get to know the culture and history of the country we visited. To finish our short stay in Dar es-Salam we went to the beach to taste the warm waters of the Indian Ocean, unknown to many of us.
We return to the airport to catch our internal flight to Mwanza, where we landed at 9:30 p.m. on 11th March. There, our hosts pick us up with a bus to transport us to Shinyanga, where we arrived after 2 p.m. The hotel they have chosen for our stay is very pleasant, with spacious and comfortable rooms, bungalow type, with air conditioning and WiFi connection (although it started to work on the thirdday of our arrival). There are a garden area and terrace for outdoor dining, which allowed us to have very nice dinners next to our well-deserved beers after the long days of work.

The next day we finally arrived at the Shinyanga hospital, 3 days after our departure. There, Dr George, surgeon in charge of coordinating the mission, and Dr Onesmo, who has been in charge of recruiting patients, await us. With them we began to coordinate to start operating patients as soon as possible.

We are informed that each patient (except children under 5 years of age) must pay 80,000 TZS (approximately 29 euros) for hospital and personal expenses. In addition, there are waiting for us 2 inspectors of the TDFA (Tanzanian Food and Drugs Authorithy), who review all the material for hours, confiscating everything they do not consider adequate (sutures recently expired) and withdrawing medication with an expiration date nearby.

Meanwhile, we started reviewing patients and scheduled the first surgeries. Once all the material was placed and the operating room was prepared, we began to operate that same day in the afternoon. We settled in one of the 3 operating rooms available in the hospital, to operate in two tables separated by a screen.

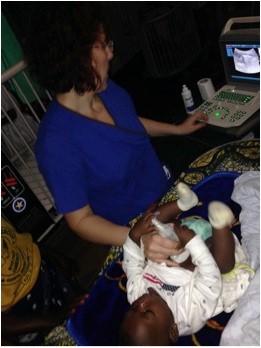
One for children and one for adults. And so we began a very hard campaign, working about 14 hours every day. The selection made by Dr Onesmo was excellent, it was only necessary to review some patients with diagnostic doubts and some pediatric patients. Approximately 18 patients were operated daily, with a lot of effort and dedication from our team, who every day gave everything to carry out all the daily work, including Sergio, our photographer, who did an accelerated nursing assistant course. The collaboration on the part of the native staff was quite deficient, although I must emphasize the enormous collaboration of Dr Onesmo, Dr Nelson, Simon (anesthesia technician) and of course, Ezequiel, who did everything on their part to help us. The work days were so intense, that we didn´t have any time to know the city, only the surroundings of the hospital and the hotel. Every day they served us the lunch in a hospital room. The food was good and plentiful.

After 5 and a half days of intense work, we are ready for our return. Again driving to Mwanza, with a tyre puncture included in the middle of nowhere. At the airport they open all the packages before entering and check all the material, despite having all our permits in order.
Finally we arrived in Madrid after 10 days of travel, with a strange feeling. Maybe we could have done better, maybe we could have operated more, but the conditions were what there were, and things don´t change in one day. I hope that in future campaigns, all the problems that were presented to us in this first mission in Shinyanga, can be solved and thus be able to carry out more useful campaigns in a hospital with a lot of potential.
After a month of our return, after which I had contradictory feelings regarding this mission, I only have in mind the good things, the smile of the children when giving them a toy or a simple caress, with their parents grateful for our help, and all the patients that we have improved their quality of life after our passage through Shinyanga. In the end this is the essence of this work. And of course, in my mind there is always the team spirit, the union that occurs between the group, especially in the difficult situations that have been presented to us. Without a doubt, this has been essential for the development of this mission and the reason why there is always a desire to repeat a mission . ASANTE SANA.
TECHNICAL MEMORY:
PARTICIPANTS:
Ana María Gay Fernández, general surgeon Álvaro Cunqueiro Hospital, Vigo
Pablo Lozano Lominchar, general surgeon Gregorio Marañón Hospital, Madrid
Lucía Garrido López, 4th year resident of general surgery Álvaro Cunqueiro Hospital, Vigo
José Miguel Morán Penco, pediatric surgeon, Quirón Salud Hospital, Cáceres and Badajoz
Beatriz Revuelta Alonso, anesthesiologist, University Healthcare Complex of León
Almudena Ceballos Ruano, nurse, Poniente Hospital, Almería
Sergio Sánchez Agullo, photographer
DURATION: Departure from Madrid 9th March 2018, arrival in Madrid 19th March 2018.
RESULTS OF THE CAMPAIGN:
Adult surgeries: 44 patients. 50 procedures.
Inguinal hernias: 34
Eventrations: 3
Hydroceles: 5
Epigastric hernias: 5
Sigma volvulus: 1
2 reinterventions for hematoma.
Pediatric surgeries: 34 patients, 41 procedures
Inguinal hernias: 15
Umbilical hernias: 5
Cryptorchid: 4
Phimosis: 5
Hydroceles: 1
Burn Cures: 3
Other procedures: 8
THE HOSPITAL:
It´s a large hospital, with 3 operating rooms and several rooms for hospitalized patients, for men, women and children separately. They have a sterilization room with an autoclave. The cleaning of the hospital and specifically the operating room area is very poor. In addition, the operating room area has many windows, which are permanently open, with the consequent entry of insects and dirt from the street.
SURGICAL MATERIAL:
-They don´t have any electric scalpel generator that works correctly, neither terminals and plates.
– They have a lot of surgical equipment, although quite old and rusty. Some boxes for laparotomy are in good condition, but the material for hernia surgery is very poor. They don´t have specific material for pediatric surgery, because children are not routinely operated in this hospital.
-they have gowns and surgical covers, but not enough for daily surgeries that are performed in this type of campaigns, so it´s convenient to include gowns and surgical fields, as well as gauzes and antiseptics.
-they have a lamp on each operating table, but light cuts due to overload are frequent, so it is advisable to wear a frontal light.
– Pediatric patients with severe burns are taken care of daily, so it´s important to take material to make cures of this type
ANESTHESIA MATERIAL:
-The hospital is equipped with a modern anesthesia machine and an older one, one in each operating room. We used the most modern one, to be able to do pediatric anesthesia. It consists of two vaporizers: one of halothane and the other of sevorane. They only have halothane, but for future missions it is good to know, for the possibility of getting sevorane and use it. The oxygen was in bottles, and they have enough for surgeries that were performed
-With regard to the medication for general anesthesia, there are muscle relaxants such as succinylcholine, ketamine and little else, so it is important to carry everything we consider necessary.
– Endotracheal tubes, aspiration probes, after being asked repeatedly, appear. There aren´t laryngeal masks.
-Fluids, systems for intravenous lines are available,
-We work in two tables in the same operating room, as already mentioned. At one table we made adults and in the other one children with the respirator. There are also several oxygen concentrators, so it is possible to use them if necessary.
-Staff local, there are no anesthetists trained as such. They are anesthetic technicians, who perform mainly spinal anesthesia, but also general anesthesia when surgery requires it. They have a great capacity to adapt to the situations that are presented to them, taking into account the means at their disposal and the little accessibility to the best in our speciality. They listen everything we told them and try to use devices like masks, which they have heard but have never seen. Their collaboration was essential to carry out the mission given the large volume of patients we had.
In summary, and although there are some material and medication, it´s preferable to take anything that we can think we need. In addition to this, the expense that we can cause over the days is diminished.
ASPECTS TO IMPROVE:
-cleaning conditions of the operating rooms. It is necessary to place mosquito nets in all the windows.
– train local staff in asepsis and antisepsis, as there are many aspects that are unknown or poorly practiced.
– help from local staff to expedite the entry and exit of patients to the operating room and then to the room.
-correct identification of patients and their clinical history.
-include patients who don´t have the financial resources that have been required in this campaign.
Ana Gay
Team Leader