L I B E R I A 2 0 1 7
2nd Slovenian “Hernia International Foundation” Expedition
Ghanta City, November 11th – 19 th 2017

This year’s planned charity mission led the Slovenian national team to Liberia, to Ghanta City and to Ghanta’s “Esther and Jereline Koung Medical Centre” (E&J MC).Our team consisted of 10 members: 3 surgeons, 3 assistants, 2 anaesthesiologists, 1 radiologist and 1 nurse.
We travelled to Monrovia with the dutch airline KLM via Munich and Amsterdam, with a short stop in Freetown. In the capital, Dr. George’s team picked us up in the middle of the night with a couple of powerful 4-wheel-drive vehicles. There were two reasons for a one hour delay at the airport in Monrovia: 1 piece of lost bagagge and a missing customs’ approval for importing the goods into the country. When the person authorized to “approve” the import of medical equipment to Liberia was finally reached over the telephone, we hit the road. The good thing about the 4 hour drive to Ghanta at night was the reasonable traffic conditions. On the way back we needed more than 5 hours. The road, built recently by Chinese, was a very good one and made travelling much easier.
The weather during the week was quite good: partly cloudy with frequent afternoon/night showers that we only heard because of the thin metal rooftops. The temperature of 30°C felt like 35°C and morebecause of the humidity. Accomodation at Jackies Guest House was a good decision (privacy, airconditioning, WiFi with some interruptions, a restaurant with reliable food and a minishop with all the essentials that one needs, even in the case of lost luggage). Some members decided to share a room to minimize the costs, which exceeded the costs of some airport hotels in Europe (USD 50, dinner about USD 20, breakfast about USD 10). Jackies Guest house was built and first owned by a local politician Mr. Koung and has now a new owner.
After some hours rest upon arrival, the welcoming ceremony in the hospital started with a prayer and speeches by Dr. Peter Mathew George and the hospital director. The hospital was constructed in July 2016 and was built by Mr. Koung.
All the patients for the week gathered in a big hall. The decision for the mission to start the next day was well accepted among all team members, although it was Sunday.

Short instructions to well educated local team
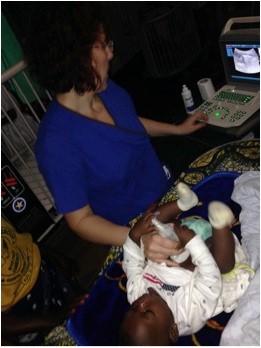
Ultrasound is allways welcome
All OT’s (0perating theatres) in the hospital were airconditioned. We had to use head lamps in just one of them, the other OT lamps functioned well. The tables were adjustable for height, which was not expected. 2 OT’s were close to each other, which made any interventions easier, especially for anasthesia. Two diathermies were working properly, there had been some trouble with the one that we brought with us. Before it is finally donated to the E&J hospital, it will be rechecked in Europe. Many thanks to Sister McDermot from South West Acute Hospital in Enniskillen, for this donation.
For the first three days, the work in all three operation theatres (OTs) ran smoothly. A special thanks goes to Dr. George, who selected the patients personally. On day four, a huge number of patients who had been waiting for surgery (almost 200) forced Dr. George to start operating himself in OT Nr. 4. This was not a very good idea from the organizational point of view as his hospital colleagues were (not yet) fully capable of recruiting and diagnosing patients for 3 or 4 OTs. Our radiologist with the ultrasound was a great help, excluding some patients (with enlarged lymph nodes, other swellings, etc.), who initially expected to be operated on.
On day four we stopped operating on children, as one of them had aspirated just recently breastfed milk during an anaesthesia induction (it took some time for the mother to understand that milk is considered as a food and not just a simple liquid). Our anaesthesiologists and the nurse managed to solve the situation skilfully with emergency drugs, an improvised aspirator and an oxygen concentrator. Under self-built intensive care, supplying antibiotics and oxygen over the following days, the aspiration pneumonia was managed and the child was saved. After this event, Dr. George took over the patient recruitment again and the mission continued smoothly. Dr. George, MD, PhD is basically an obstetrician and gynaecologist with the good skills of a general physician and is capable of performing hernia surgery, including Lichtenstein mesh repair. And of course, with organizational talent. One of his reliable co-workers, Dr. Charles might also be an important link for future missions. Emanuel, an anaesthesiology assistant, showed a lot of readiness to upgrade his anaesthesiological skills. In the absence of HI teams, the whole anaesthesia issues in the hospital depend on him

»Talking« to pediatric patients before surgery

During narcosis induction
We worked daily from 9am to 7pm, sometimes even longer. The local staff were always ready to work, even late into the evening. Lunch break (chicken gyros sandwicheslike doner kebabs, sometimes French fries with fish) was also an opportunity for briefing the morning patients and planning the rest of the day.
The good thing of having a self sufficient team (surgeons, assistants, anaesthesia,..) was to work with people that one knew from hospitals at home and that were used to working as a team. Anyway, we educated the local staff as well, among them were many very motivated volunteers who applied to work for free during the week and helped so that the mission could succeed.
As we did not have enough gloves to fully suport all the teams in 4 operation theatres in the sense of double gloving (as a Spanish team had done some months earlier), we used single gloves because of the expectation that all patients were HIV and Hepatitis B tested. As this was only possible for 2 days from the side of the hospital and further on against additional payment, we paid for the tests for the rest of the patients ourselves. It was not realistic to expect that the patients should cover these costs as they expected that the management would be free of charge. Covering some minimal costs from the side of the patients (or the hospital) is an issue that can be discussed in the future.
Anyway, the best surgical infection prophylaxis is a considerate and careful operating technique.
A good decision was to bring along over 300 disposable sterile gowns and sterile hole-drapes to ensure the sterility of the operative field. With additional education of the scrub-teams, we were more and more satisfied with the preparation of the operative field. One of the suggestions to the new hospital director Mr. Victor W. Kpaiseh (the general directors of the hospital had changed during our mission) was providing cloth gowns at least for the scrub personnel. This would demand improving the sterilization capacities (buying the second charcoal-run autoclave pot), which are one of the bottle-necks of the process. This idea is probably not immediately applicable, but might be solved in the future.


One of the incisional hernias with praeperitoneal repair
In 6 working days (4 full days, 2 half days) we performed 103 procedures on 86 patients (14 female, 72 male). The average age of the patients was 36.5 years. The oldest patient was 89 years, the youngest 1 year. The majority of patients had inguinal and large inguinoscrotal hernias (71).
Predominantly we repaired inguinals using the Lichtenstein (>95%) and sometimes the Shouldice technque with young patients (<5%). In 14 pediatric patients with inguinal hernia, the Mitchell Banks and Ferguson techniques were used. We performed 2 incisional repairs (retromuscular), 17 umbilical repairs, 2 undescended testicle repairs, 1 femoral hernia repair and 1 hemorrhoids operation (acute). We performed 2 revisions, 1 due to a postoperative haemathoma, 1 for a suspicious haemathoma (negative revision). As we had a reliable anaesthesia team, the anaesthesia was predominantly spinal (72), general (13) and local in only 2 cases.
The presence of a radiologist on such a mission was a very good idea: 70 performed ultrasound diagnostic checks preoperatively, 3 postoperative ultrasound checks, 12 pregnant women with ultrasound (education of midwives), 16 emergency ultrasounds.

Our team with the medical director of »E&J MEDICAL CENTRE«
Dr. Peter Mathew George
At the end of the team work, we agreed with Dr. George, that it was a good mission. The farewell ceremony was much more a cultural event than just saying thanks and we were thankful to be able to be in Ghanta City, Liberia, together with the local hospital staff for their patients.
All this would not be possible without a skilled, experienced and enthusiastic team:
– Tomaž Benedik (consultant, surgeon, 2nd mission)
– Maria Greiner (consultant, surgeon, 1st mission)
– Marija Jekovec (consultant, radiologist, 1st mission)
– Irena Urbancic (consultant, anaesthesiologist, 1st mission)
– Katarina Primožic (registrar, anaesthesiology, 1st mission)
– Katja Carli (registrar, surgery, 1st mission)
– Luka Kovac (registrar, gynaecology and obstetrics, 2nd mission)
– Selena Benedik (medical student, 2nd mission)
– Mateja Selic (scrub nurse, acted as an anaesthesiological nurse, Hernia International mesh sterilizing support)
– Jurij Gorjanc (consultant, surgeon, team leader, 7th mission)

