Senegal (Sédhiou), January, February 2016.
Our Senegal adventure begins on January 22nd, 2016 at 19:30 hours. We, the members of the team who are going to carry out the Sédhiou mission, have gathered in the Barajas airport. We almost all know one another. Teresa Butrón, surgeon and president, Pepe Pascual, surgeon and patron of the Foundation, María Fanjul, paediatric surgeon, Carmen Santiago, urologist, Beatriz Revuelta, anaesthetist, and Elisardo Bilbao, surgeon. Faustino accompanies us to help us with our bags and to encourage us. He also takes regular photos to preserve the images of our trip.

Boarding card in hand, and after sealing and checking our bags, we pass controls and get ready to begin a journey we all had been looking forward to. We first fly to Dakar, where Mariama Badji is waiting, and from there to Zinguichor. Then to Sédhiou, 143 km by road in about two and a half hours.
Mariama is a Senegalese reporter who had worked a long time in the Guinea embassy in Madrid. Back home she has been a great help to us, both in personal matters and in the development of the mission. His relationships within the country, the organization of official events, her help in the daily routine of administration, provisions and translations, reservations of places, her company, her advice…
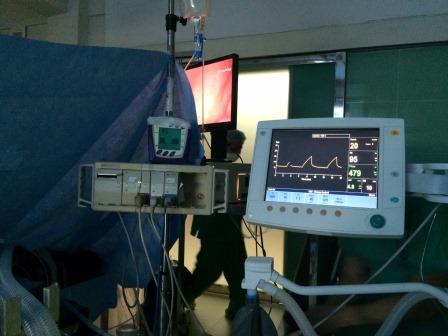
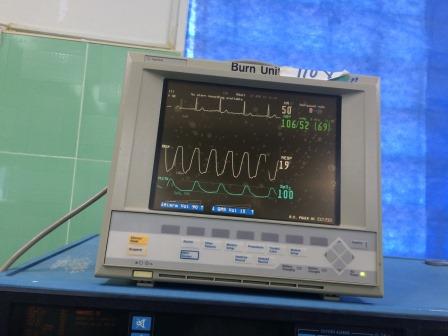
We arrived on time but tired at our destination after a long journey on 23/01/16 in the afternoon. Our first visit was to the Sédhiou Hospital where, for five and a half days, we carried out our mission. After being received by the officials of the centre, we download our cargo from the two vans from Zinguichor. We place each object in its proper place. Teresa does it with the help of the rest of the team. The operation theatre has sufficient place for our sutures, meshes, electric scalpel terminals, etc. We also place the two generators we have brought from Madrid (one of them donated by the Bilbao Red Cross) which, together with the one they have, will allow us to operate three patients at the same time. For that we place another table in the largest room and a partition to separate them from one another The ceiling light is quite satisfactory. The small room is also ready for surgery with full guaranty.
With everything in order and with the collaboration of Dr. Camara and all the rest, we give order to clean up the whole zone as we intent beginning work the next Sunday, 24/01/16.
Tired and with things still pending we decide to retire to our quarters. None of us knew where we were going to spend the night, but Mariana, once again, took care of it. La Palmarie is a hotel reserved for hunters and situated by the river Casamance, with great confort, food and good rooms. None of us had seen such luxury before. We had always have had good lodgings, but the arrangements in Sédhiou were the best we had ever seen. We were grateful for it, as it is important for us to go to work each day in good condition.

Watching before breakfast the sunrise over the river gave us sufficient energy for the whole journey. The light in Africa is different.
January 24, though a Sunday, became a working day for us. We began our work with the hospital in full swing. Three tables were ready. We distributed the work among us together with the local surgeons. This time we had three anaestesists: Beatriz, Ousman Sarr the chief, and Ousman Thiam. We checked the reports and the patients. We operated upon our first three patients and got used to the instruments there. The first day went by easily with a rest at midday with the sandwich Mariana had ready for us. Meat with onion, potatoes and eggs. That will be our menu all those days.
Monday 25 full work. We attend the first interventions of the Dakar gynecologist who has come with Mariama. Dr. Moustapha shows a great ability, knowledge and good criterion. He is anxious to learn, and prys attention to everything he is told. He is like one more in the team.
Special mention deserves the work of our urologist, Doctor Carmen Santiago, who added to her fine character her scientific training in dealing with hidroceles, and worked with the gynecologists in the correction of vesico-vaginal fistulae we found it would be worth thinking of organizing specific missions for this type of pathology that in Senegal, and particularly in poorer zones in the country, is a social problem.

Child surgery is one of the most delicate aspects of these missions. The collaboration in this occasion of Doctor María Fanjul, of great energy and solvency, solved this problem for us. A good companion, she enjoyed more than any the relaxing baths in the swimming pool at the end of each day.
That this mission has been important and should be repeated regularly is established by the interest shown by the official institutions in the Sédhiou department. On January 26 we attended a reception prepared for us by the civil and religious authorities of the region presided by the governor himself. He, together with the mayor of the city and the director of the hospital and of health stressed the importance of such collaboration, not only for the direct action on the largest number of patients, but also for the possibility of informing local doctors and nurses in techniques for hernias, which are very frequent, and often turn out to be mortal, in the area. The president of the Foundation answered with a few words of thanks and her offering international cooperation right from now. The effect of our expedition was enhanced by the interview that the RTS1 (public TV in Senegal), made to one of the members of our team, Elisardo Bilbao, and which was relayed at state level 5 times on successive days.
The 27th began as usual. Part of the team visited those operated upon on the previous day and exploring new patients, and the rest began operations. We worked simultaneously on three tables, and this was possible thanks to the coordination by Doctor Beatriz Revuelta, helped by Doctors Saar and Thiam. Her serenity, her permanent smile, and her camera always ready enlivened our work and will help us to keep good memories of it. The anaesthetist is in such situations indispensable in every way. One day we were able to see film seven vultures “analising” samples of pathological anatomy…
One of the most touching acts of our stay took place in the afternoon. After work and showers we were taken to the “Casa de la Cultura” in the city. Together with the governor and the local authorities, we enjoyed local music by a small group. We came to know the instruments, songs, and verses. They even showed us their dances. It was unforgettable. Each of us was given a diploma by the Health and Public Affairs Ministry. The ladies were dressed in their best with full elegance, while us…
Work is intense and occasionally with unforeseen complications. South of Senegal there is a serious problem with vesico-vaginal fistulas. Some women become mothers when they are still girls, and they suffer for life many anatomical hurts, with the consequence for family and society life and exclusion from them. That is why the arrival of a team with gynecologists and urologists encourages such patients to come. Unfortunately we we could only solve some cases as others would need a greater specialization. It would be interesting to organize special missions for such problem exclusively.
What with one thing and another part of our team returned to the hotel on the 28th after 23.30 hours. We were worried about the impossibility of communication. We called the hospital director who came from his home to the center and told us he had left the operation theatre late and would be arriving shortly. Senegal is a safe country, but there are accidents, chiefly on the road.

January 29th was in theory our last working day there. We had to finish early as our translator, Mr. Sankoun Gassama, had invited us to his home in the Boraya island, where we enjoyed a crab dinner prepared by his family. The crossing of the Casamance River was done on a boat full of people (more than sixty crowded together) with their goods, hens, cattle etc. They risk their lives desperately seeking a hypothetical paradise, and this is very sad. We were very well received and we visited the village chief who expressed us his thanks. We sat down in a semicircle to share in their prayers. Back home and surrounded by children we took again our boat in darkness thanks to the expert pilot who took us to the landing place where we were not seeing anything.
The last day of our stay we saw again all the patients we had operated upon and we gave their leave to those whose wounds had healed. We operated on one more patient, and Dr. Camara on another one. All together 74 patients (13 of them children) with 89 procedures in six days. The predominant pathology was inguinal hernia, followed by epigastric hernia, a good number of hidroceles, most of them giant ones, and vesico-vaginal fistules, some anus wounds, skin tumours, etc. We were happy we were a multi-discipline team and could share experiences with learning on both sides, which made our mission a very successful one.
But all comes to an end, and we have to look forward to new missions. We have found an extraordinary human team, ready to work and eager to learn. Farewells are always mixed feelings, chiefly when one has shared so much and so intensely.
We had our last meeting in the director’s office with all the hospital team and the local Health Chief where we examined our work and looked forward to future missions taking into account the present needs, particularly the treatment of fistulae.
Then the family photo and the trip by car to Zinguichor in a hurry as the drivers had to go back before the road would be closed for curfew as that zone at that moment was occupied by independent rebels who, though controlled at that moment, they still could threaten our way. Our trip of about two hours was uneventful. Mariama had reserved for us the Aubert Hotel where we enjoyed full comfort and commented on all our experiences.
On the 31st at 7.30 am we were at the airport to fly to Dakar at 9, arriving an hour late. After leaving all our luggage in the house of Mariama’s brother and resting for a time, we went to the harbour to take a ferry fo the Goree Island, from where slaves started for America for centuries.
The bilingual guide we engaged took us round the island and to a restaurant where we had our meal. In the afternoon the most interesting thing was our visit to the slaves house. It was a painful experience. The way the overfed them so that they would weigh more than 60 kg, the punishments to those who protested with flogging and even death, the abuse of women, chiefly of virgins, the contrast with the quarters of the bosses on top of the jail itself overwhelmed us. Whatever you read about this will never approach the reality of the awful vision.
Buck to our boat we were taken to a painter’s workshop where they showed us how to draw a picture with only resin and sand with spectacular results.
We disembarked and went to a market near the harbour where we bargained, bought, got tired and finished up our adventure.
After collecting our luggage from Badji’s house we went to the airport to come back to Madrid with the satisfaction of having carried out our mission and the sorrow to have to leave back such marvelous persons, with the intention to come back as soon as we have another occasion.