TANZANIA 2 0 2 2

Hernia International Foundation
Slovenian-Austrian-Swiss (Liechtenstein) Team Mission
Malya, Tanzania March 20th-26th 2022

Click here to view video
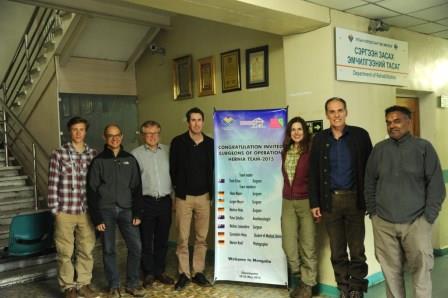
Malya Village with its Health Center (MHC) was host for a Hernia International (HI) mission for the first time in its history. The reason for the mission was Dr James Marco, a skilful and ambitious surgical resident, who was inspired by HI-charisma after visiting the village of Momella during our 2019 mission.
The week-end travel from our homes to Malya HC took us 32 hours and even 42 hours for some of us. Three consecutive flights from Vienna (Zürich) to Doha, Kilimanjaro (Arusha) and an internal flight to Lake Victoria (Mwanza) were followed by an almost 3-hour jeep ride from Mwanza to MHC. Unfortunately we had to fly without our experienced anaesthetist Dr. Michael Wirnsperger, who was Covid-19 positive some days before departure.

Our team consisted of 5 members: 2 surgeons, 1 radiologist, 1 scrub nurse and 1 nurse anaesthetist. Additionally, surgical consultant Dr. Avelina Temba, Rev. sister of our Lady of Usambara from Korogwe joined us for two days and her presence enabled us to import medical equipment without notable delay. It should be emphasized that every HI-team travelling to Tanzania in the future should apply for importation of ALL medical devices and drugs at the TMDA website online at least 3 months before the mission to avoid serious bureaucractic issues at the airport. We imported 205 kg of equipment and drugs in 12 bags. No additional fee for excess luggage was payed at the Zürich airport thanks to Manuelas’ negotiation skills and her past Red Cross connections.

Checking patients for surgery was the first task on Sunday evening and Monday morning. As MHC is a village, far away from civilization, patients came every single day after they were informed via posters, local radio and social media. Every single day, there were just enough patients for 1 day, not too many, not too few. The youngest patient was 1 month old, the oldest had 90 years.
The turnover of the patients was fluent. We were not used to taking a lunch break, but biscuits, water and delicious cashew nuts were sufficient between operations. Besides performing operations on hernias (numerous recurrent and scrotal), assisting the local doctors and nurses was high on our priority list. We took time to do this as education and teaching might be of at least as much importance as performing the operation itself. Local doctors (Dr Temba, Dr James Marco and Dr Mchemba) became more independent and self-confident under our supervision.
Parallel operations on 2 tables, including suspending hernia operations to give precedence for Cesarean sections (performed by local doctors), enabled 46 procedures on 38 patients in 4,5 days.
Dr Rems (experienced consultant, past chief surgeon and hospital director) and I were happy to see grateful patients and improved surgical technique of local surgeons. Wolfgang, a skilled nurse anaesthetist from Feldkirch, Austria was completely souverain in performing general anaesthesia in patients of all ages and built a trustful team with the anaesthesia staff at Malya HC (medical officers William and Mathias). For our scrub nurse Manuela from Lichtenstein, this was the 4th international mission, after serving in Cameroon and on Red Cross combat missions to Syria and Bangladesh several ears before. Once again, the presence of an experienced radiologist turned out to be a reasonable decision. Marija performed 41 US-exams, including in OB-GYN and on our surgical patients pre- and sometimes postoperatively. Due to the high mean age of patients after inguinal hernia repair under spinal anaesthesia, US check on evenings post operatively was a routine in elderly patients (average age of adult inguinal hernia patients was 58 years). Due to untreated benign prostatic hypertrophy in some of these patients, unrecognized urine retention post spinal anaesthesia might be an underestimated but serious issue in commonly forbearing and compliant patients. In these cases we performed urinary catheterization and gave adviced on further management.

Good work in the hospital was also possible because we were accommodated well in the christian MMCT Guest House (bed, breakfast and dinner). Malya HC might not be able host additional hernia missions in the near future, as Dr James Marco is moving to the Ngudu District Hospital, 33 km away. But a visit of the surgical chief of staff Dr Misana from that hospital brought us a new invitation. They have great need and abundancy of patients. Mesh surgery is not performed in that remote part of Africa at all, compared to hospitals and health centers of our last missions (Korogwe, Arusha).

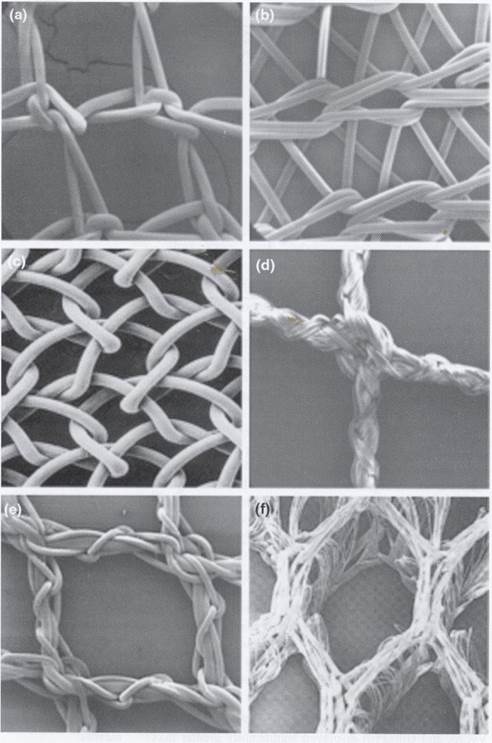
Among 38 patients (with 46 procedures), we operated on 5 children (13%) and 33 adults (87%). 7 patiens (18%) were female. The most frequent diagnosis was inguinal hernia (29 pts, 76%), followed by Jabouley`s procedure for hydrocaele (8 pts, 21%). In inguinal hernias in children, Mitchell-Banks repair and in teenagers and young adults a 4-layer Shouldice procedure was performed; Lichtenstein repair with LDPE mesh was performed in theevast majority of patients with inguinal hernia. In incisional ventral hernias, the sublay procedure was the method of choice. We performed 1 orchidectomy in a patient with a giant hydrocaele and testicular atrophy. Other diagnoses/operations were for acute appendicitis, mastitis in a newborn (extremely rare according to published data), abscesses, undescended testicle, benign breast lesions and skin tumors. We placed suction, corrugated or Penrose drains after almost all operations on big incisional and scrotal hernias, and some hydrocaeles. Our anaesthesia team also helped in Cesarean section.
In OT 1 (good lights, we brought diathermy), mainly general anaesthesia was performed, while procedures in OT2 (no surgical lights, without diathermy) we used spinal and local anaesthesia.

We felt privileged for having no complications (minor or major) which we attribute to a not overcrowded programme. Again, we took enough time for every single procedure, without any hurrying. Good working and a friendship-building atmosphere was a result of mission preparation several months before, not to mention sister Avelinas attitude and prayers throughout the mission as an additional factor.
Team Members:
Dr Miran Rems – consultant surgeon, Jesenice, Slovenia
Dr Jurij Gorjanc – consultant surgeon, team leader, Austria & Slovenia
Dr Marija Jekovec – consultant radiologist, Ljubljana, Slovenia
Manuela Logan – scrub nurse, Grabs, Switzerland & Lichtenstein
Wolfgang Walser – anaesthesia nurse, Feldkirch, Austria
Our sponsors:
Medical Center Gorjanc
Implantoloski institut / Implant Institute
Hospital of St. John of God St. Veit/Glan
Krankenhaus St. Vinzenz Zams
LKH Feldkirch
Spital Grabs
Kirurgija Bitenc University Medical Centre Ljubljana