REPORT on VISIT to HEBRON HOSPITAL
PHNOM PENH, CAMBODIA
for
HERNIA INTERNATIONAL
24th April-1st May, 2015
……………………………………
Surgeons: Prof. R. David Rosin (Barbados)- Team Leader
Dr. Ramesh Jonnalagadda (Barbados)
Mr. John Payne (United Kingdom)
Anaethetist: Dr. Michael Platt (United Kingdom)
Nursing Officer: Mrs. Jacqueline Platt (United Kingdom)
Unlike previous Hernia International missions, our hosts were not interested in volume of operations undertaken, but more in training & teaching. It was therefore agreed that we would teach their young surgeons the standard Lichtenstein inguinal hernia mesh (using mosquito net) repair each morning in the Operating Rooms & run Basic Surgical & Anaesthetic Skills in the afternoons. The latter was made possible by the generous loan of equipment by Mr. Martyn Coomer, Head of Research at the Royal College of Surgeons of England.
We were met at the airport by the hospital administrator, Stephen Kim, who aided us without any problems through customs with surgical instruments, which we donated to the hospital, as well as the teaching equipment, sutures & other aids. The team stayed at three different hotels in the city. One of the biggest problems in Phnom Penh is travelling around the city as the traffic is thick with thousands of scooters & tuk-tuks weaving their way through the cars. The traffic problems stem from little public transport. The Hebron hospital is situated near to the airport but some way from the centre of the city with all its sights & restaurants.
BACKGROUND to CAMBODIA
History: Peoplehave been living in what is now present dayCambodia at least since the 5th century BCE. The ancient kingdom of Funan occupied a wider area & the culture became heavily influenced by Hinduism. This was followed by the Chenla Empire (6th century – 802 ACE) & then the Khymer Empire which had its golden age between the 9th & 13th centuries during which time Angkor Wat was built.
As in many countries there followed the Dark Ages from 1431 – 1863 & was under the suzerainty of Vietnam. It then became a protectorate of France being ruled as part of Indo-China. The monarchy remained in place & they as well as many of the leaders were educated in France. The French ruled until the Japanese occupation during the 2nd world war, during which time thousands of Cambodians died. The French ruled again after the defeat of the Japanese until 1953 when King Norodum Sihanouk declared independence back by the Geneva talks. In 1970 Lon Nol ruled the country & the King fled to France. Lon Nol was replaced by Pol Pot & the Khymer Rouge in 1975 when they entered Phnom Penh. They ruled for 4 horrendous years during which >2 million people were slaughtered or died in captivity from starvation- the “killing fields”. They were overthrown by the Vietnamese who occupied the country until 1993 during which time it was called the Peoples Republic of Kamputhia. Meetings were held between 1991 & 1993 in Paris to agree on an independent Cambodia with the King as a titular head. However, civil unrest continued until 1997 when the present day Cambodia took shape. It covers an area of 180,000 Sq. Kms, has >14,000 villages & a population of 14+ million people of whom 20% are urban. The GDP/Capita is given as $1,000 with a growth rate of 6.5%.
BACKGROUND to HEBRON HOSPITAL
It was founded by Protestant missionaries (<2%of the population is Christian) from Korea & opened in 2007 with 3 medical doctors & 1 dentist. At that time it was purely an outpatient based unit though clinics were also held in the provinces. In 2010 the hospital was extended with in patient wards, operating rooms, heart services, an eye centre, a cancer centre & regular staff training in Korea. Clinics were also held in Laos & Myanmar.
The present facility comprises- 3 well equipped operating rooms, a recovery room, an Intensive Care Unit, 70 inpatient beds (only 40 were being utilized during our visit), an endoscopy suite, a radiology unit, department of pathology, dental & eye clinics, a library, auditorium, board/teaching room. Chapel & nursing college. The medical staff includes 5 general practitioners, 1 ophthalmologist, an internist(Korean), an orthopaedic surgeon(Korean), 2 pathologists(Korean) & 3 part-time clinicians, a surgeon, an anaethetist & a physician (all Korean). There are 11 trainees. The dental unit has 2 dentists & an hygienist. There are 2 pharmacists (Korean) & 12 Korean volunteers. The nursing staff include a Head Nurse (Korean) & 16 nurses. Support services include 7 people in the laboratory, 2 opticians, 2 medical engineers, & 2 physicists. Administration (as seems universal) was well staffed with 13 people.
The hospital would be classified as a Day Hospital in the UK being an elective unit though emergencies are accepted during the day being seen in the clinic or admitted directly to a ward. The Hospital opens at 0500 hours by which time there are usually >200 patients waiting in an outside seated covered area. The clinics commence until 0730 when there is a half hour meditation time followed by another half an hour entitled preaching time. Ward & operating work commences at 0830 until noon when all work ceases for an intersessionary prayer time & lunch. Apart from a skeleton staff on the wards the hospital is closed until 1400. The day ends at 1700 hours by which time >300 outpatients have been seen 94% of whom are Cambodian.
The case load has increased dramatically from 2007 to 2014. In 2007 5,000 patients were seen, 1,000 investigated in the laboratory & 4,000 prescriptions given. 7 years later these figures reached-53,000 patients seen, 28,000 investigated & 40,000 prescriptions written. The surgery covered most specialties comprising 34% orthopaedic, 28% plastic, 16% ophthalmology,21% general, with 1% gynaecology & ENT surgery.
Cambodian fertility rate are 2.5/female; household size 4.7; infant mortality rate 40/1,000 number of doctors 2.3/10,000 & number of nurses 7.9/10,000 population. We were informed the cost of medical services was broken down as health care 31.25% public, 26% private & 12.7% non-medical with transport costs accounting for 6%.
The Hebron Hospital sums up its role as a) providing medical care, b) educating future medical Christian leaders, c) caring for missionaries & d) supporting the local churches. To this end they are extending the hospital by a further 100 beds.

PROGRAMME at HEBRON HOSPITAL
Day 1, Friday 24th April.This was an orientation day. We had a tour of the hospital which is a 60 bedded hospital with 40 beds in use. The foundations were being built for enlargement by an extra 100 beds. We visited the wards, theatres (3 well equipped operating rooms), endoscopy unit, out-patient clinic, auditorium & lecture/ board room. We were introduced to the Senior Anaethetist, Dr. Kim Jae Seon, who spoke good English, the Senior Surgeon, & the Pathologist (one of two consultants in Phnom Penh) who had trained in New Zealand. The staff were a mixture of Cambodian & Korean Doctors. Jacqueline Platt met with the Senior Nurse & theatre nurses.
After a midday service in the entrance hall, we had lunch with the staff, enjoying typical Korean fare (photo 1). We learnt that there was an enforced siesta every day from 1200 to 1400 hours. We then had two lectures, the first on the hospital by Stephen Kim & the second on Cambodia by Dr. Seon. Following this we were informed that the hospital did not perform elective work at the week-ends so we would start work on the Monday. However, they had arranged for the patients on whom we were to operate to come to be examined by us in the wards. With an unexpected free week-end, Ramesh, an avid golfer, discovered Stephen played golf. We thus arranged for Ramesh, Mike, Stephen & myself to play very early on the Saturday & to visit the “Killing Fields” on the Sunday. I managed to visit the exquisite Royal Palace as well on the Sunday afternoon.
Day 2, 27th April.We arrived at the hospital early to discover that nothing really started before 0900 hours. We did another ward round & then briefed the theatre staff about our intended operations, Mr. Payne & Mrs. Platt introducing them to the WHO guidelines on “time out” prior to commencing any operation.
Three operations were performed, all inguinal hernia repairs. One was repaired under local anaesthetic, a large irreducible hernia under GA & the third case started under LA, but found to be a sliding hernia, so was converted to a GA. After lunch, Dr Platt helped in a pain clinic. Mr. Payne, Dr. Ramesh instructed 12 trainees on the basic surgical skills of knot tying & instrument handling. Lectures were delivered on “The Past, Present & Future of Surgery” by Prof. Rosin” & on “The WHO Guidelines” by Mr. Payne. A post-operative ward round was carried out & patients for the following day reviewed.
Day 3, 28th April.
Due to heavy rains during the night we were collected an hour late & our journey to the hospital took a further hour so we did not arrive until 0900. We carried out a post-operative ward round as we found the patients from the previous day were still on the wards (the staff were reluctant to discharge patients) as well as seeing patients for the morning lists & marking the appropriate sides as necessary.
Once again only 3 operations were arranged-2 inguinal hernias & an umbilical hernia all children & all operated on under general anaesthesia. During the morning a young woman was admitted with peritonitis. I discovered they had a unused laparoscopic stack so agreed to laparoscope her after lunch.
Dr. Ramesh & Jacqueline Platt were released to see the Royal Palace. During the afternoon Mr. Payne taught the trainees on further basic surgical skills whilst Dr. Platt & myself operated on the lady with peritonitis. She had a purlent perforated appendicitis so I was able to perform a laparoscopic appendicectomy with extensive peritoneal lavage. Dr. Platt then helped in the pain clinic whilst I joined Mr. Payne teaching. Instrument handling & interrupted suturing was taught & practiced. I gave a lecture on “The different approaches to Inguinal Hernia Repair with videos on Laparoscopic TAPP & TEP repairs”. Prior to departure our usual post-operative ward round was carried out.
Day 4, 29th AprilWe arrived early to find 4 children with hydocoeles, 1 young boy with a phimosis & 2 inguinal hernias were scheduled. Also Dr. Platt had agreed to deal with 8 pain patients for blocks under C arm control. The post-operative patients were seen & the patients for the day’s operating were also seen & the relevant sides marked. The 5 children were all operated on under GA & the 2 adults with inguinal hernias under LA. During the afternoon Dr. Ramesh performed a mastectomy for an advanced breast cancer whilst Dr. Platt dealt with his pain patients & Mr. Payne & myself took the afternoon teaching session which was devoted to all types of suturing followed by lectures from Mr. Payne on “The Management of Haemorrhoids” & a further one on “Anal fissures & Fistulas”. At our post-operative ward round I was delighted to find that the lady who had undergone the laparoscopic appendicectomy for peritonitis had bowel sounds present.
Prior to our departure Stephen had found out that it was my birthday & presented me with a cake & candles & collected all the staff to sing Happy Birthday to me. Unfortunately Drs. Ramesh & Platt had not been informed about this & were drinking coffee in the operating suite talking to the staff.

Day 5, 30th April
Only 2 patients were scheduled for surgery. A young man with an irreducible inguinal hernia & a bilateral inguinal hernia on whom I had agreed(providing he was a suitable candidate) to perform the surgery laparoscopically. However he did not show up for the operation so only one operation was performed after our ward round. We started the teaching session early with lectures on “Soft Tissue Injuries” & “A Clinical Quizz” from Dr. Ramesh & on “Different Types of Anaesthesia” & “Pain Management” from Dr. Platt.
Discussion with the trainees & feed back was carried out by Drs. Ramesh, Platt & myself. The trainees informed us that they had never been taught any surgical skills previously & they thoroughly enjoyed the sessions, asking us to stay on to carry out more. We were gratified to hear that 8 of the 11 first year trainees now wanted to become surgeons.
The day ended with the presentation of a tribute to the team from the staff at Hebron by Stephen Kim. A speech was given by Dr. Seon & a reply on behalf of the team by Professor Rosin.
David Rosin
Report of Anaesthesia and Pain Management performed by Dr Michael Platt in Phnom Pen
April 27 – May 1st 2015

My wife Jacqueline (a seasoned senior nursing sister currently working with Health Education England) and I (a seasoned anaesthetist and Pain Medicine specialist), arrived in Phnom Pen on April 22nd and checked into the Dara Airport Hotel in the centre of the city. The Dara Airport is a modern hotel with large rooms and excellent dining and spa facilities, and superb air conditioning (very necessary in 43 degree Celsius heat!).
After spending a few days familiarising ourselves with the city, meeting up with the surgeons, David Rosin, Ramesh J, John Payne and their wives, we spent Friday at the Hebron Hospital where we were due to work, as part of a Hernia International programme. Here we were introduced to the hospital: a small but very modern hospital with two floors, the operating theatres and wards being on the 1st floor, clinics downstairs on the ground floor. The hospital is funded by a South Korean Christian organisation called ‘Jesus Cambodia’. It was reasonably well supplied and had the latest anaesthetic machines, sterile surgical gloves and most of the equipment needed for straightforward surgery and anaesthesia (including sevoflurane anaesthetic vapour.

I performed general anaesthesia for the more difficult patients, and one elderly gentlemen who was not coping with local anaesthesia.
The age range was 11 months to advanced elderly. All were remarkably fit and posed no anaesthetic problems. All the patients received local regional analgesia, giving excellent post-operative analgesia. All the patients received intravenous cannulae in the pr-operative ward prior to surgery, with Normal Saline solution running as they came to theatre. All the patients were anaesthetised using propofol intravenously, maintained on oxygen and air with sevoflurane via facemask or LMA.

It was on the second day of operating that our hosts discovered that I was also a pain medicine specialist and asked me to see some difficult patients for them. The first patient was actually the wife of one of the surgeons who had recently had a knee replacement operation but was getting much pain in the lateral aspect of the knee at the Fibular/Tibial joint. I injected this with some steroid and local anaesthetic under x-ray guidance. The pain immediately abated and she was able to mobilise much more easily. Of the seven further patients I saw, they included knee pain in soccer player (reassurance and encouraged to exercise); cervical disc prolapse with C8 radiculopathy (x-ray guided nerve root injection plus cervical epidural with steroid and local anaesthetic), Two patients presented with lumbar L5/S1 radiculopathy (x-ray guided nerve root injection and epidural); An elderly lady presented with symptoms and signs of lumbar spinal stenosis (but no MRI available, so she was treated with epidural, requiring admission for weak legs, but fully recovered by next morning with no pain. Two patients had hand issues with evidence of some arthritis, relived by injection and prescribed exercises. It seems there is no formal physiotherapy available in Phnom Pen currently.
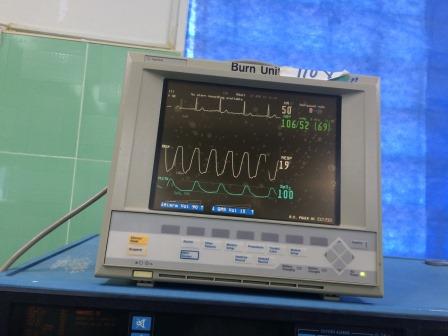
My wife worked with both myself and the nurses, encouraging them and demonstrating some modern nursing techniques and help with some of the more difficult patients to nurse. We also introduced to them the WHO surgical checklist, encouraging them to use it routinely and to increase their safety processes. I was very impressed by the standard of care, the standard of anaesthetic assistants, many of whom had been trained overseas including in Australia. It was a very fulfilling week working with a keen workforce and teaching some very keen young doctors who are all anxious to help patients in the best way they can. In addition to the work, we spent every afternoon teaching, involving both lecture/tutorials and practical teaching. I attach several photographs illustrating the anaesthetic equipment and monitoring, clearly to a surprisingly high and modern standard.
I would highly recommend the experience, and I would be happy to return.
Michael Platt