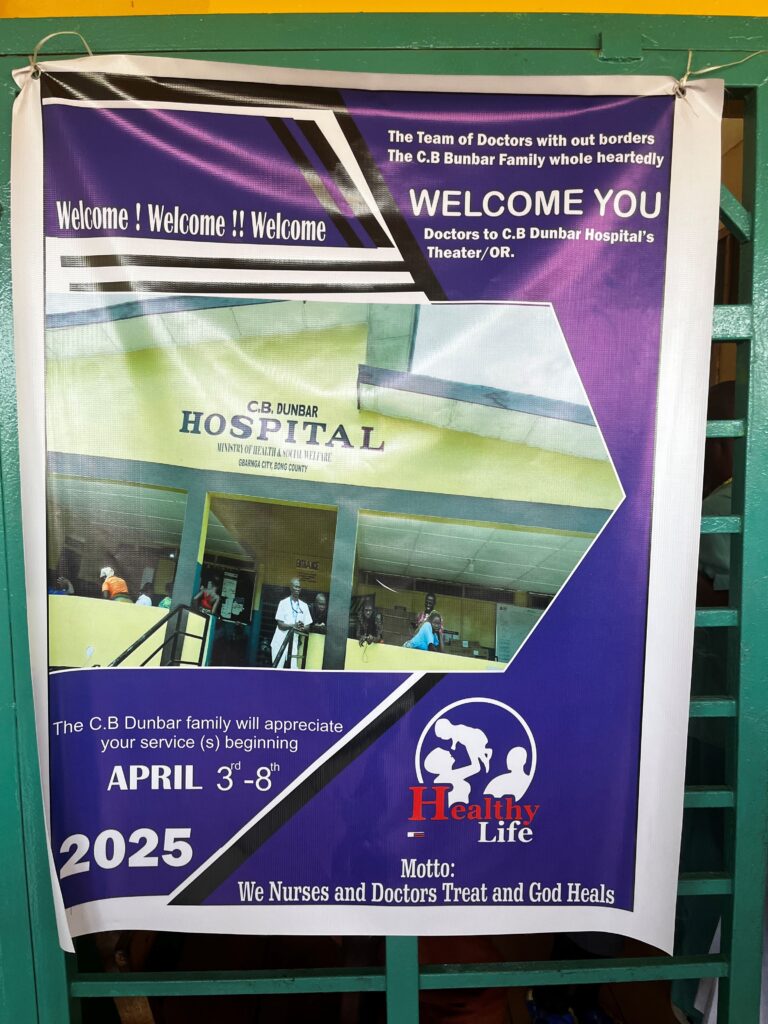
Campaign District Hospital Kwimba-Ngudu. Tanzania
Dates: Saturday 29th March to Sunday 6th April 2025.
1. TECHNICAL REPORT:
1.1 DATES AND LOGISTIC DEPLOYED:
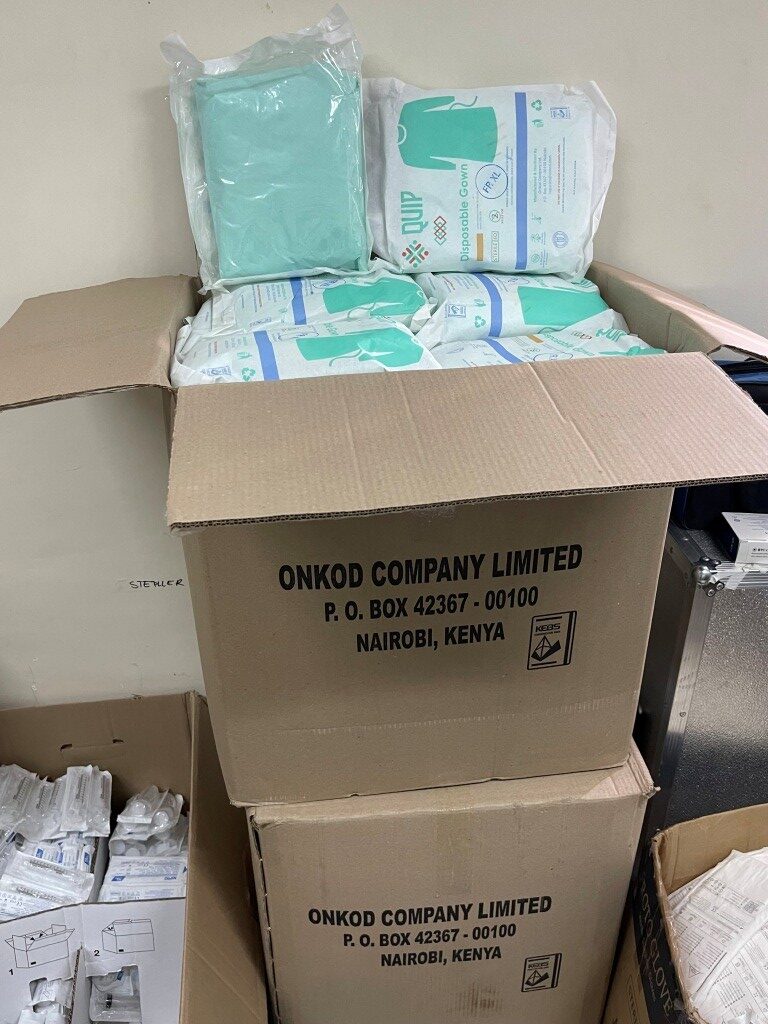
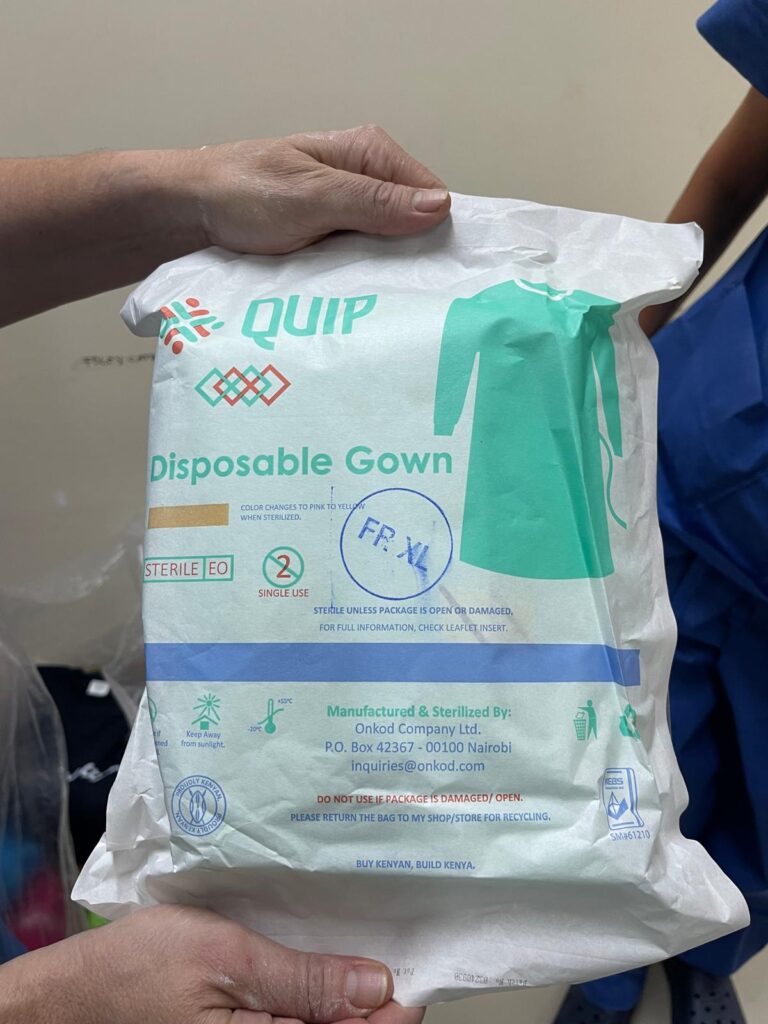
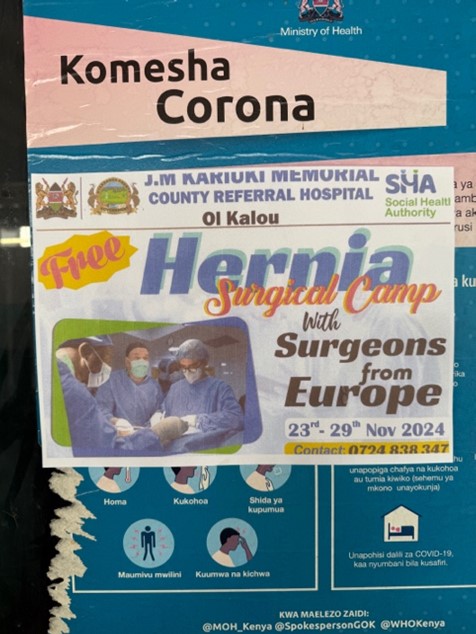
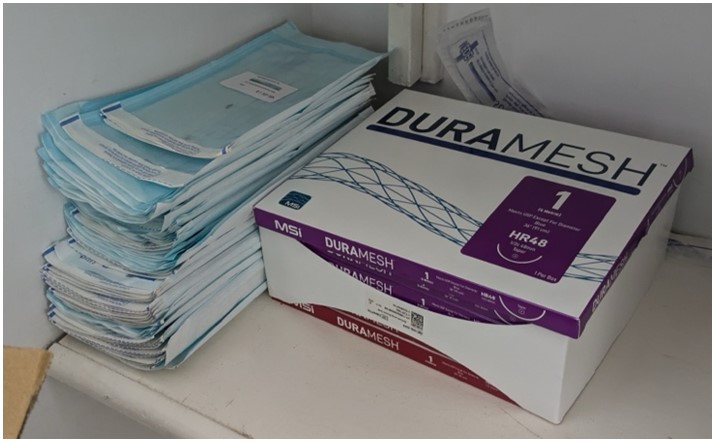
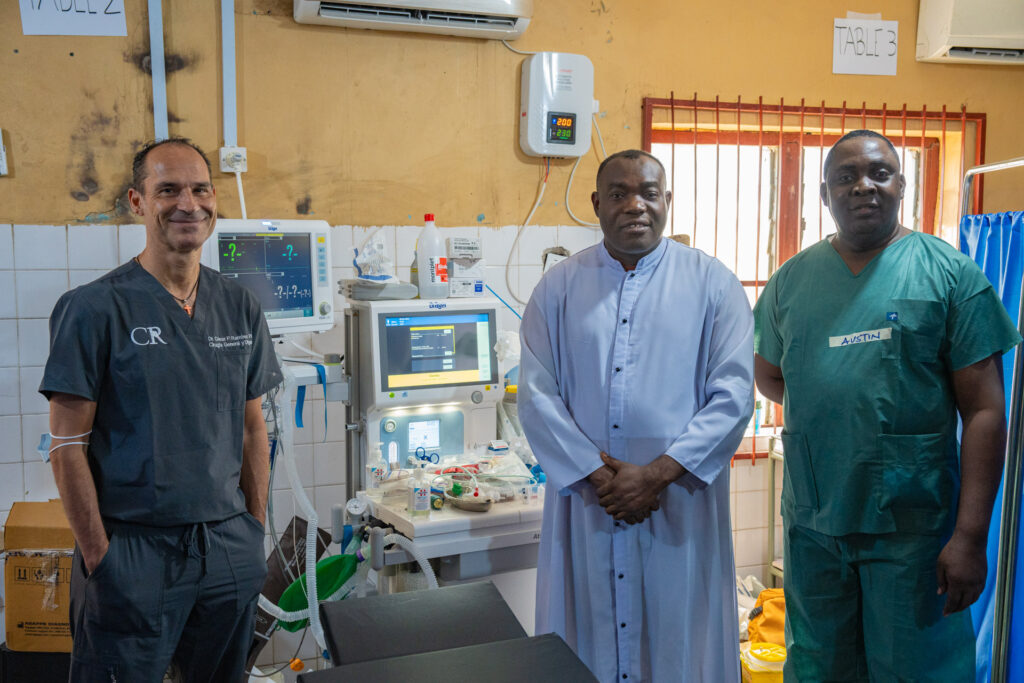
The team of cooperants began training in early November 2024, coordinated by Santiago García del Valle and assisted by Dr. Teresa Butrón, director of the non-governmental organization Cirujanos en Acción, and under the umbrella and collaboration of the Hernia International Foundation. A team of 12 people was formed, including pediatric and adult surgery, anesthesiology, and nursing. This was the first campaign that Cirujanos en Acción has organized at the Kwimba District Hospital. The team of volunteers was responsible for collecting all the consumables needed for the campaign, including surgical gowns, sheets, sterile surgical drapes, sutures, meshes of different types and sizes, urinary catheters, sterile and non-sterile gloves, as well as a large quantity of drugs (general anesthetics, local anesthetics, muscle relaxants, antibiotics, opioids, analgesics, etc.) and disposable anesthetic material, including spinal and regional anesthesia needles, laryngeal masks, and other necessary materials.
Dr. Violeta Heras brought a portable ultrasound device that was very useful for performing regional block techniques for postoperative pain. Dr. Lourdes Delgado provided a significant amount of oral medications for postoperative analgesia in pediatrics.

The plane tickets were obtained through Angelis, who works as a “free agent” for the Halcón Viajes agency. The tickets were purchased from Turkish Airlines, which allowed the transport of one 30-kilogram bag per person plus carry-on luggage up to a total of 10 kg. However, we didn’t encounter any problems at the Madrid airport when we exceeded this amount. In fact, Turkish Airlines donated medical supplies they had on their premises. The journey included stops in Istanbul and Dar Es Salaam, from where a local flight took us to Mwanza. We were greeted by staff from Kwimba Hospital (Dra Mogassa). After loading our equipment into two cars, we were taken to our accommodation in Ngudu after a two-hour journey. It is worth highlighting the fact that the planes that operate local flights from Dar Es Salaam to Mwanza are small and have limited cargo capacity, so half of the equipment had to be transferred on a later flight and collected at the airport.
Our initial contact in Tanzania was Dr. Marco James, although in the last month he was transferred to another health district and Dr. Elizabeth Mogassa was our reference person. This contingency made the final communication somewhat difficult and slowed down some of the necessary procedures for the development of the campaign.
There was no difficulty in obtaining the necessary visas and permits to carry out our task. The Tanzanian customs authorities request a certificate of donation of the material to be moved, as well as a list with the approximate estimated value of each product and the estimated expiration date. We forwarded these documents to Dr. Mogassa. At customs, after some discussions, we were allowed to pass all the material with the help of an individual letter of invitation from the Kwimba Local Government authorities

1.2 ADULT PATIENTS:
The following procedures were performed in adults:
– 15 inguinal hernioplasties
– 1 umbilical hernioplasty
– 2 supraumbilical or epigastric hernioplasties
– 1 paraincisional hernia
– 14 large lipomas
– 1 fibroid
– 2 giant ovarian cysts
– 1 emergency hysterectomy
– 2 cesarean sections
– 1 epididymal cyst
– 1 hemorrhoidectomy
– 1 Axillary abscess evacuation
– 1 excision of multiple perineal condylomata

1.3 PAEDIATRIC PATIENTS:
In the pediatric population, the following procedures were performed:
– 3 umbilical hernias (2 hernioplasties and 1 herniorrhaphy).
– 3 inguinal herniorrhaphy
– 1 Removal of supernumerary finger of hand
1.4 TOTAL PROCEDURES:
A total of 50 surgical procedures were performed
1.5 TOTAL PATIENTS:
A total of 45 patients were operated on.
1.6 COMPLICATIONS:
A patient, pregnant at term, came to the emergency department with a retained dead fetus and had to undergo fetal extraction and urgent total hysterectomy with the help of local staff. She died hours after the operation due to incoercible haemorrhage and puerperal sepsis.

A wall hematoma occurred after hernioplasty. She did not require more than surveillance and compressive bandaging.
There were no other major complications during our hospital stay nor were there any other complications 15 days after our departure from Ngudu.
2. REPORT OF THE CAMPAIGN
2.1. THE PLACE
Kwimba is one of the seven districts of the Mwanza region and its most important population center is Ngudu. It is located in the northwest of Tanzania and the nearest airport, two hours away by road, is the one in Mwanza, on the shore of Lake Victoria, although it does not receive international flights. It is a very rural area, with very small urban centers, including Ngudu, being agriculture the main occupation of the population, generally carried out on small family plots. Agricultural work is carried out from December to May and this fact was definitive in explaining the little surgical activity performed, as many potential patients were unwilling and unable to leave their livelihood until harvesting the year’s crop, thus foregoing surgery at that time.

The District Kwimba Hospital is located about 7 kilometres from Ngudu and, as we were informed, serves a population of about 70,000 people living in isolated houses or small rural villages in an area that stretches for many kilometres with difficult transportation and therefore difficult and costly access to the hospital for a large part of the population. It is a single-story building, located in the countryside. It is spacious, with a very rational layout and has emergency, hospitalization, pediatrics and gynecology wards, with very little surgical activity except for cesarean sections.
2.2. THE TEAM

Paediatric surgery
Lourdes Delgado Cotán.
Adults General surgery
José Manuel Hernández González.
Patricia Maldonado Valdivieso.
César Lévano Linares.
María Savoie Hontoria.
Irene Ferrer Vilela.
Anesthesiology
Violeta Heras Hernando
Susana Rodríguez Giménez
Santiago García del Valle (Team leader)
Nursing
Yolanda Gómez Pérez
Elena Iñiguez Mentxaca
Mónica Pérez Ortiz

2.3. LOCAL STAFF
In the absence of Dr Marco James due to relocation, Dr Elizabeth Mogassa was our local contact and put us in touch with the hotel and the catering company.
In the hospital there are 3-4 general practitioners (General Practitioners) dedicated to surgical activity, led by Dr Haruna Elias who perform caesarean sections as they arise. The anesthesia of these patients, almost exclusively spinal, is performed by nurses who perform the technique well but lack the necessary knowledge to deal with possible complications
2.4. EQUIPMENT
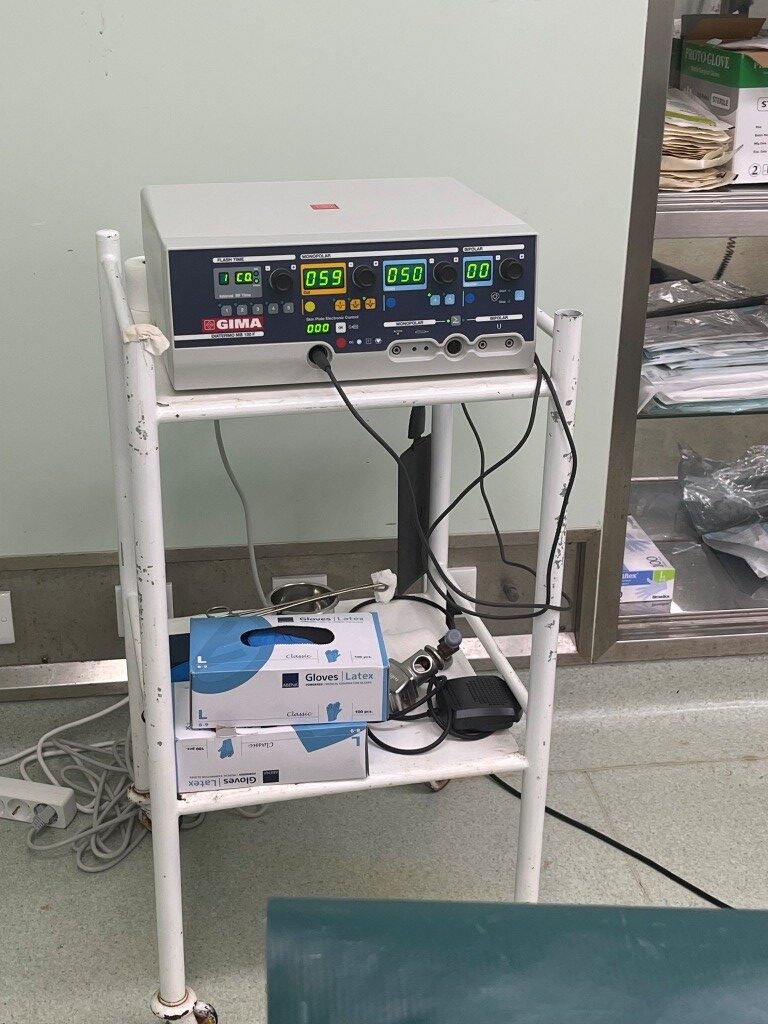
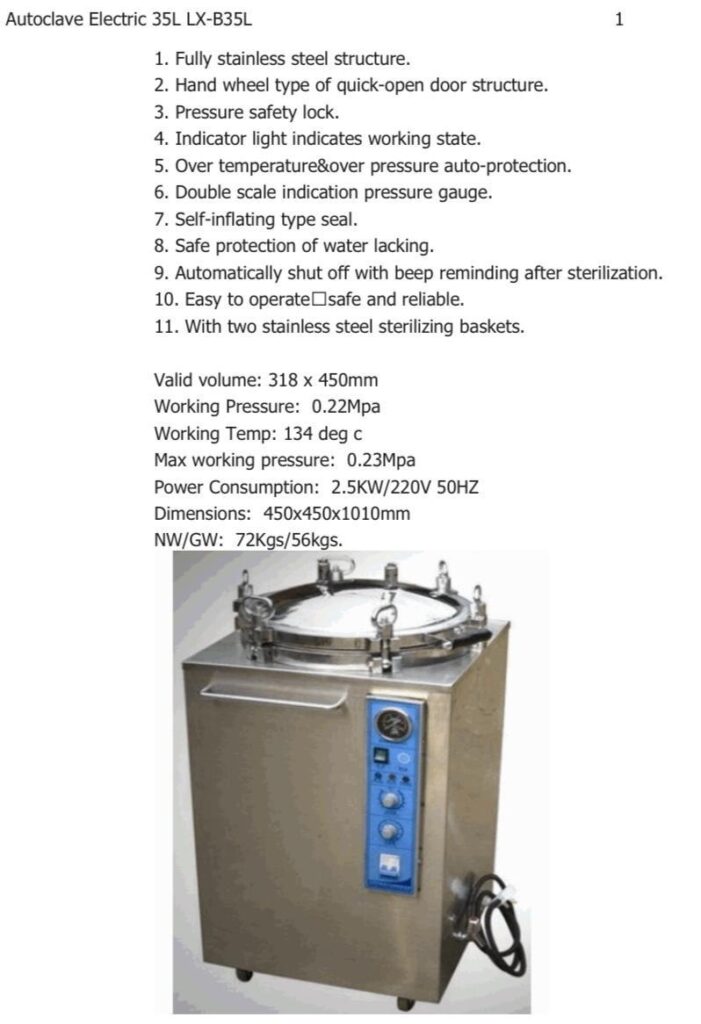
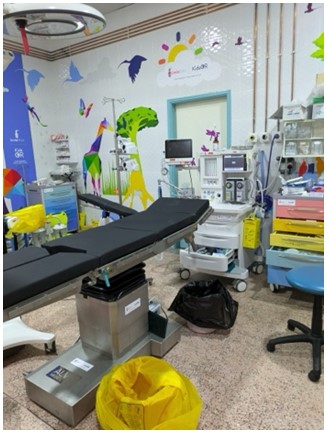
The hospital has two adjacent operating rooms of small size, insufficient to be able to install two tables in one of them. In addition, they use one of the two operating rooms for cesarean sections, generally urgent, a situation that happened to us between 2 and 3 times a day which meant pausing our surgical activity. In addition, there is a small room in the emergency room that can be used for minor surgery or wound care under local anesthesia. Although we bring instruments from Spain, they have enough material and sterilization systems. They have some drugs (Propofol, local anesthetics, ephedrine, oxytocin, etc.) but no narcotics or muscle relaxants. There are no diathermy generators so we had to transfer two sets of equipment from Spain.
There is a small resuscitation room with space for 2-3 patients with an SpO2 monitor
2.5. ANAESTHESIA
Most procedures in adults were performed under spinal anesthesia supplemented later with ultrasound-guided blocks (ilio-inguinal or transverse abdominal plane block). In children they were performed under general anesthesia with laryngeal mask and always supplemented with regional block for postoperative anesthesia.

In each of the operating rooms there is an anesthesia machine, old but perfectly operative, with Halothane and Isoflurane as anesthetic agents. There is monitoring of basic operative parameters in each operating room. There is no centralized gas (Air, Oxygen, N2O), only large capacity oxygen cylinders connected to the anesthesia machines. There are oxygen concentrators and suction devices but of low power.

It has the capacity to cross (whole) blood and transfuse, an aspect that we were able to verify since a patient undergoing an emergent obstetric hysterectomy required units of whole blood
2.6. ASEPSIS AND SURGICAL MATERIAL
It has the capacity to sterilize surgical instruments and surgical linen equipment.
In the same way, it has a good amount of surgical instruments that we complement with material donated by Dr. César Lévano
2.7. OUR LIFE IN NGUDU.
We stayed at the PAM Lodge Hotel in Ngudu. Single rooms, clean and spacious. There is no hot water. The night, accommodation only, cost about US$10 per day. The hotel is adjacent to a bar or discotheque and on party days the music would go on late into the night making it difficult to rest.
All the catering was contracted with a small company formed by local women who prepared breakfast and lunch in the hospital itself and dinner was served in a dining room of the hotel.
At 7:00 am we were picked up at the hotel and transferred to the hospital where we had breakfast with the rest of the operating room staff. The first two days of the campaign was the Tanzanian National Holiday so there was almost no activity at the hospital. Although Dr. Mogassa assured us that an appeal was made in the weeks prior, there were very few patients ready to be evaluated, most of them showed up at the hospital during the days we stayed in Ngudu. As the days went by we were able to operate on a greater number of patients, but always fewer than we would have wished.
At 14:00-14:30 our food was brought to us: various types of vegetables, salads, rice, chicken, fruit, always hot and generally well prepared. In the afternoon we continued to operate until finishing around 19:00-20:00 in the evening. Dinner was served in a room of the hotel around 21:30.
As the surgical activity was not very intense, we visited some schools and talked to the teachers informing them about the possibility of assessing children and young people with hernias or other medical problems.
The group of volonteers returning directly from Kwimba had to suffer the cancellation of their flight from Dar Es Salaam to Istanbul. Although they were able to be reassigned to another flight, they suffered the inconvenience of a long waiting time in Istanbul. Although they complained to Turkish Airlines, to date, they have not received the requested financial compensation.
A group of the team extended their stay in Tanzania to visit some national parks near Mwanza (Ngorongoro, Tarangire, etc)
3. CONCLUSION
3.1 STRENGTHS OF THIS PLACE:
1.- The local staff, both doctors, nurses and auxiliary staff, are very involved and actively participated with us, helping in all tasks.
2.- Very acceptable facilities
3.2. IMPROVEMENT OBJETIVES:
1.- Prior recruitment of patients. This task was practically not carried out and made our work very difficult. Improve the previous information of the campaign to the population.
2.- Since there are many transfers and local flights in small planes, it is advisable to adjust the displaced material to the scheduled activity, which is linked to the previous point.
3.- Adjust the dates of the campaign. Schedule it outside the agricultural work season, ideally between May 20 and June 30.
4.- To be able to have a local generator (they had two units but none of them worked) would facilitate our work.
5.- The trip to Ngudu was very long and with several long stopovers and road transfers. I suppose it will not be easy to optimize the times, but it is important to have the dates well in advance and the teams formed to ensure that the stopovers will be of the shortest possible duration.
4. BUDGET:
4.1. COST PER PARTICIPANT:
VISA: 80 euros
Flights: 850 euros
Accommodation and meals: 160 euros
4.2. CAMPAIGN TOTAL COST:
12.900 euros
5. FIRMAS
Fdo: Santiago García del Valle
Responsable of the campaign
Cirujanos en Acción