Hernia International Mongolia May 2025
The team consisted of 3 volunteers from Australia (Rob Bohmer, Andrew Zhang, Hairul Ahmad) and 1 from Bulgaria (Dragomir Daranov), from 26 May to 6 June 2025. The first week was in Darkhan, a provincial town of about 100 000 population, the second largest in Mongolia. The second week In Ulaanbaatar Second General Hospital. The trip was well organised locally by Dr Enkhee and Dr Sonor, who sorted all out paperwork, registration, transport and hotel bookings (WhatsApp the preferred method of communication).
The work experience
In Darkhan, the team conducted 22 operations, mainly incisional and inguinal herniae but cancelled 11 patients. The cancellations were due to poor optimisation/selection (cirrhotic patients, patients on blood thinners, asymptomatic patients, smokers, overweight patients or frailty). There were 2 available theatres but not well utilised, starting often at 930am and long change over times. With 4 visiting surgeons, local surgeons and 2 theatres, there was a lot of waiting around. A new laparoscopic stack arrived while we were there, providing excellent vision however the sutures and scalpel blades were poor quality and some of the hand instruments need replacing. The surgeons were keen to learn and generally were excellent technically but need to work on pre-op selection and optimisation of the patients. A harmonic scalpel was available! There is an ICU but staffed at times by the anaesthetist on call who had to do 2 jobs at the same time. Case selection in terms of safety needs to be considered, although liver resections are now being offered there. We provided all the mesh used, all other equipment was locally provided.












In Ulaanbaartar the team conducted 20 operations, again mainly incisional and inguinal hernia, some large and complicated from liver surgery. Again 13 were cancelled mainly due to poor selection and optimisation. An attempt was made to get the local surgeons to operate on all cases and see the patients with us pre-op (the latter more difficult to organise but should be a priority for future missions). The laparoscopic equipment was good as most surgery is performed this way including lap gastrectomies and lap liver live transplant harvesting has just started in the hospital! The surgeons are technically excellent, however pre-op selection and optimisation could be improved. “Time out” and sharps handling could be improved especially with a high incidence of hepatitis. Post-op care seemed good but we only saw the patients on day 1 or 2 post-op and have not been involved in longer term complications such as mesh infection. We provided all the mesh used. Component separation and TAR release was often required for the complex herniae.



The visitor experience
The local surgeons, residents and staff involved with our visits were amazingly friendly and hospitable and we thank them, often they teach us more than we teach them. Inter-country work is a privilege and contributes to surgery in so many ways apart the technical side of surgery. Thanks especially to Drs Naraa and Sonor, residents “George” and “Jenni” who interpreted for us.
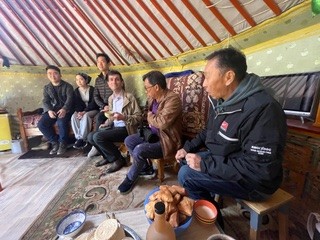
Most surgeons understand some English but are shy to speak it. We were hosted very well in both places, taken to dinners, treated to a local music show and taken to the country to experience farm life in rural Mongolia. Vodka and beers flowed at times! Both hotels we stayed at were of high standard.
Recommendations for future teams
Mongolia has made a huge advancement in laparoscopic surgery since I was there 7 years ago and in Ulaanbaartar, do mainly laparoscopic work including inguinal herniae. They are keen to progress their skills which means Hernia International should select surgeons with advanced abdominal wall reconstruction experience. The local surgeons need to clearly state what they need from visiting surgeons to allow for the best experience for them and the visiting team. Saying that, the local surgeons really appreciate any input from visiting surgeons to ensure they are up to date with world standards. Although the local surgeons are skilled and keen to learn new techniques, equipment can be difficult to get hold of and may not be in the best working order (including lap needle holders and limited suture options). Mesh is now available more readily but patients seem to have to contribute to the costs. Mesh for the visit was provided by the visiting team. Botox is not available. Visiting surgeons need to be adaptable and weigh the balance between teaching new techniques and being aware of safety issues this can raise. Pre-op assessment and patient optimisation should be a key teaching issue. “Time out” posters are in theatres but not often practised, promulgating this would be another way visiting teams could improve safety in surgery in Mongolia. Sharps precautions should be worked on. The junior staff work long unsafe hours. The surgeons have a government stipulation that any “urgent” surgery needs to be done within 2 hours, supporting the local surgeons to change this so appendicectomies and cholecystectomies do not usually need to be done after midnight would be useful and improve patient safety.
Patients were seen in rooms with multiple people popping in and out, privacy not an issue! It would be best to insist on seeing patients with a surgeon present rather than a resident only, to talk about the decision process. The theatre lists frequently changed without the visiting team being notified. There is a significant time spent sitting around as only 2 theatres were available in both hospitals, 4 visiting surgeons and emergency cases bump hernia lists.
We would suggest, the first morning should be set aside for a talk about the weeks plan and who is going to operate each day, discuss operation plans and the types of mesh available, basic anatomy and pre-op optimisation rather than leave it to the end of the week lecture. Maybe Ulaanbaatar should be the first week, with the first morning teleconference shared with the country hospital and visit the country hospital second week. We would suggest a local surgeon coordinates theatre flow and the Hernia International surgeons role for each case and ensuring sufficient mesh supplies for each case. Where possible a local surgeon rather than resident should interpret to improve decision making. Overall a very rewarding experience and thanks to all the local surgeons and people involved.
Rob Bohmer

